Sonographic Screening for Down Syndrome
Dr. Fergal D. Malone
Director Obstetrics and Gynecology Ultrasonography,
Associate Professor Columbia University of Physicians and Surgeons,
Columbia Presbyterian Medical Center, New York, NY (USA)
Screening for Down syndrome is an important part of routine antenatal care. Significant advances have been made in antenatal screening for Down syndrome over the past few decades. The most common screening method in the United States involves the assessment of a combination of factors: maternal age, multiple second-trimester serum markers, and second-trimester ultrasonography. More recently there has been significant interest in first-trimester methods of screening, including screening for first-trimester markers and the sonographic measurement of fetal nuchal translucency. Invasive prenatal diagnosis for Down syndrome with amniocentesis or chorionic villus sample (CVS) is offered only to women of advanced maternal age (older than 35 years at delivery) or those who previously had an affected child or to women who has abnormal multiple-marker serum screening. The most efficient multiple-marker screening test in the second trimester is the "quad" screen, comprising alpha-fetoprotein (AFP), human chorionic Gonadotropin (hCG), unconjugated estriol (E3), and Inhibin-A. This approach yields sensitivities for Down syndrome of 67-76%.
The purpose of the document is to summarize the current data and shift toward first-trimester screening for Down syndrome.
Fetal Nuchal Translucency:
Nuchal translucency refers to the normal subcutaneous fluid-filled space between the back of the fetal neck and the overlying skin. Sonographic criteria to maximize quality of nuchal translucency sonography are:
- Nuchal translucency ultrasound should only be performed by sonographers or sonologists trained and experienced in the technique.
- Transabdominal or transvaginal approach should be left to the sonographer's discretion, based on maternal body habitus, gestational age, and fetal position.
- Gestation should be limited to between 10 weeks 3 days and 13 weeks 6 days (approximate fetal crown-rump length, 36-80 mm).
- Fetus should be examined in a midsagittal plane.
- Fetal neck should be in a neutral position.
- Fetal image should occupy at least 75% of the viewable screen.
- Fetal movement should be awaited to distinguish between amnion and overlying fetal skin.
- Calipers should be placed on the inner borders of the nuchal fold.
- Calipers should be placed perpendicular to the long axis of the fetal body.
- At least three nuchal translucency measurements should be obtained, with the mean value of those used in risk assessment and patient counseling.
- At least 20 minutes might need to be dedicated to the nuchal translucency measurement before abandoning the effort as failed.
Nuchal translucency ultrasound measurement at 13 weeks in chromosomally normal fetus measuring 1.6 mm. Various features of good nuchal translucency ultrasound technique are evident in this image: adequate image magnification, midsagittal plane, neutral neck position, inner-to-inner caliper placement perpendicular to the fetal body axis (as indicated by white arrow), and separate visualization of the overlying fetal skin and amnion.

Malone, First Trimester Screening, Obstet Gynecol 2003.
There seems to be a direct correlation between increasing nuchal translucency measurement and risk of Down syndrome, other aneuploidies, major structural malformations, and adverse pregnancy outcome. There are several hypotheses regarding the pathophysiology of large nuchal translucency, and it is unlikely that a single common etiology for this sonographic sign underlies all associated abnormalities. Possible etiologies include cardiac failure secondary to structural malformation, abnormalities in the extracellular matrix, and abnormal or delayed development of the lymphatic system.

Increased nuchal translucency measurement of 3.7 mm at 12 weeks in a fetus with Down syndrome.
Malone, First Trimester Screening, Obstet Gynecology 2003.
Nuchal Translucency Screening with First Trimester Serum Markers: Combined Testing
Research in first-trimester maternal serum screening has consistently shown that pregnancies with fetal Down syndrome are associated with higher levels of total hCG and of the free beta subunit of hCG (with a median multiple of the median [MoM] of 1.83 in affected cases) and lower levels of pregnancy-associated plasma protein A (with a median MoM of 0.38 in affected cases). These first-trimester serum markers seem to be independent of nuchal translucency, which would imply that both serum and ultrasound approaches can be combined into a single protocol more effective for screening than either alone. The overall sensitivity for Down syndrome from various studies is about 82% for a 5% false-positive rate. A normal first-trimester screening result is about one fifth as likely in the absence of Down syndrome (negative likelihood ratio 0.18, 95% CI 0.14, 0.24).
Nuchal Translucency Screening with First- And Second-Trimester Serum Markers: Integrated Testing
Incorporating nuchal translucency and maternal serum markers obtained in the first trimester with maternal serum analysis from the second trimester to provide patients with a single risk assessment has been proposed as an alternative to quoting separate Down syndrome risks in each trimester. This two-step approach, commonly known as the integrated test, involves combining nuchal translucency and pregnancy-associated plasma protein A in the first trimester with serum AFP, hCG, unconjugated E3, and Inhibin-A in the second, with a single Down's risk result being provided in the second trimester. The advantage of this test seems to be a very high sensitivity for Down syndrome, with models suggesting that this might be as high as 94% for a 5% false-positive rate.
Nuchal Translucency Screening and Ductus Venosus Flow in the First Trimester:
In addition to nuchal translucency measurement, first-trimester sonographic evaluation of ductus venosus flow has been described for aneuploidy screening. Forward biphasic pulsatile ductus venosus flow (as illustrated in picture below) is normal, whereas reversed flow at the time of the arterial contraction has been associated with aneuploidy and heart defects. 59% to 93% of aneuploidy fetuses in various studies have shown abnormal first-trimester ductus venosus flow velocities. It has therefore been suggested that after completing a nuchal translucency ultrasound examination, further study of the fetal ductus venosus flow velocity waveform might be useful to modify a patient's risk for aneuploidy. This could be used either to improve the detection rate of nuchal translucency alone or alternatively to reduce the false-positive rate.
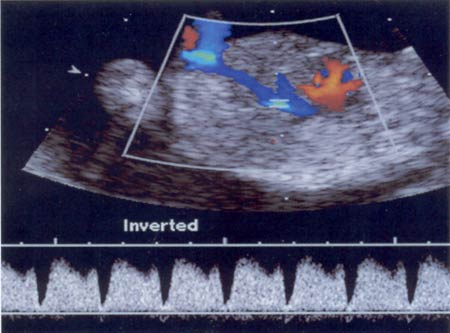
Ductus venosus flow velocity waveform in a normal 13 week fetus. The Doppler gate is placed in the ductus venosus between the umbilical venous sinus and the inferior vena cava. Note that there is biphastic pulsatile flow with constant forward flow. The troughs of flow during the atrial contraction also demonstrate forward flow.
Malone, First Trimester Screening, Obstet Gynecol 2003.
Nuchal Translucency Screening And Nasal Bone In The First-Trimester:
It has recently been suggested that absence of the fetal nose bone on first-trimester ultrasound screening is associated with increased risk for Down syndrome. Adequate imaging of the fetal nasal bone can be technically challenging in the first trimester, and careful attention to correct technique should therefore be paid to ensure consistency in technique. The nasal bone should be visualized on ultrasound along the midsagittal plane with a perfect fetal profile. The fetal spine should be down, with slight neck flexion. Two echogenic lines at the fetal nose profile should be visualized; the superficial echogenic line is the nasal skin, and the deeper echogenic line represents the nasal bone. This deeper echogenic line representing the nasal bone should be more echolucent at its distal end.
Nasal bone image of a euploid fetus at 13 weeks' gestation. Various features of good nasal bone technique are evident in this image: a good midsagittal plane, clear fetal profile, downward-facing spine, slight neck flexion, and two echogenic lines, representing the overlying fetal skin and the nasal bone. The white arrow represents the fetal nose bone, which loses its echogenicity distally.

Malone, First Trimester, Obstet Gynecol 2003.
Nuchal Translucency Screening in Multiple Gestations:
It seems that the nuchal translucency distribution does not differ significantly in singleton compared with twin pregnancies, which implies that the Down syndrome detection rates should be similar. The false-positive rate of nuchal translucency screening might be higher in monochorionic twins because some complications unique to monochorionic gestations, such as twin-to-twin transfusion syndrome, might present with increased nuchal translucency measurement. Although additional approach on the efficacy of this screening method in multiple gestations is still needed, nuchal translucency measurement should at least represent an improvement over serum screening in multiple gestations. Currently, some centers are already using nuchal translucency sonography to assist in selecting fetuses for reduction in higher-order multiple gestations.
Implementing Nuchal Translucency Into Clinical Practice:
Nuchal translucency sonography has pushed prenatal screening for Down syndrome into the first trimester, and might lead to major advances in prenatal care. Initial training in nuchal translucency sonography, however, is only one element of the quality control needed to optimize this technique. Systems must also be put in place at each local ultrasound practice to ensure that ongoing quality assurance is maintained. Mean nuchal translucency measurements increase by approximately 17% each week from 10 to 14 weeks' gestation. Therefore it is inappropriate to use a single millimeter cutoff to define an abnormal nuchal translucency or a pregnancy that warrants invasive fetal testing. More appropriate options include using the 95th percentile for a particular gestational age or MoMs. Further studies are needed to evaluate the role and feasibility of center-specific or sonographer-specific medians in a national Down syndrome screening program.
Second-Trimester Ultrasound for Down Syndrome:
Nuchal translucency screening does not obviate the need for second-trimester ultrasound for the detection of structural fetal abnormalities. Common pathologic and sonographic features of Down syndrome (trisomy 21) are: nuchal thickening; cystic hygroma; non-immune hydrops; hydrothorax; brachycephaly; epicanthic folds; short nose; round, low ears; broad neck; protruding tongue; mild ventriculomegaly; cardiovascular malformations - VSD,ASD,PDA; duodenal atresia; esophageal atresia; anorectal atresia; omphalocele; echogenic bowel; undescended testis; mild hydronephrosis; widening of iliac wings; clinodactyly; short upper and lower extremities; increased space between first and second toes.
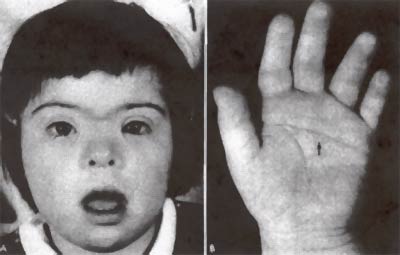
A. Photograph of a 3 year old girl, showing the typical facial appearance associated with Down Syndrome. B. The typical short, broad hand of this child shows the characteristic single transverse palmar crease (arrow). Summary:
With the increasing range of Down syndrome screening tests available to obstetric providers today, there is a need for accurate comparative data to evaluate the best combination of tests to implement into practice. First-trimester screening seems to derive much of its efficacy by combining nuchal translucency with pregnancy-associated plasma protein A and free beta subunit of hCG evaluation. An integrated screen, incorporating nuchal translucency and pregnancy-associated plasma protein A in the first trimester, together with AFP, hCG, unconjugated E3, and Inhibin-A in the second trimester, seems to be the single most efficient test. The comparative performance of each type of screening, by fixing each test at an 85% Down syndrome detection rate is summarized in the chart below:
Variation in false positive rates for a fixed 85% detection rate for Down syndrome according to the method of screening. NT= nuchal translucency; AFP= alphafetoprotein; hCG= humal chorionic gonadotropin; PAPP-A= pregnancy-associated plasma protein A. Informed consent regarding the variety of prenatal screening tests for aneuploidy should be an integral part of the screening process itself. Because of complexity of choices regarding the different screening options, and because of the range of abnormal outcomes associated with increased nuchal translucency, it will be vital to provide all patients with pretest genetic counseling before embarking on these newer forms of screening. Some patients might be most interested in the earliest possible screening result; for such patients, combined first trimester nuchal translucency and serum screening might be desired. Other patients might be most interested in the most efficient test, maximizing their detection rate and minimizing the need for amniocentesis; for such patients, a single integrated screen result combining first and second trimester approaches might be desired. Still other patients might not present for care sufficiently early to take advantage of first trimester screening; for these patients, there should be the option of second-trimester serum screening and genetic sonography.
Malone. First Trimester Screening. Obstet Gynecol 2003
Dedicated to Women's and Children's Well-being and Health Care Worldwide
www.womenshealthsection.com


