Syphilis in Pregnancy: Prevention of Congenital Syphilis
WHEC Practice Bulletin and Clinical Management Guidelines for healthcare providers. Educational grant provided by Women's Health and Education Center (WHEC).
The World Health Organization (WHO) estimates that each year maternal syphilis is responsible for 460,000 abortions or stillbirths, 270,000 cases of congenital syphilis and birth of 270,000 low-birth-weight or premature babies. This toll easily exceeds that of other neonatal infections, such as human immunodeficiency virus (HIV) and tetanus. Syphilis during pregnancy is generally low in developed countries; it ranges from 0.02% in Europe to 4.5% in the parts of the United States. There has been dramatic incidence of congenital syphilis in rural areas of Eastern Europe and Central Asia. High rates of syphilis (3-18%) have been reported at antenatal clinic in Africa, where congenital syphilis may account for about 1% of admissions to pediatric wards (1). Congenital syphilis should by now be a medical curiosity. Its continued occurrence is a symbol of the failure of basic systems of antenatal care and control of sexually transmitted diseases (STDs).
The purpose of this document is offers recommendations for treating infants and adults. It will also high-light the need to view syphilis screening and control programs through the perspectives of multiple stakeholders so as to identify barriers to, and opportunities for improving the formulation and implementation of national policies. Devising an effective political strategy might represent one of the most challenging facets of implementing a sustainable program. Both structured and unstructured approaches are useful, and applying aspects of both may provide rich analysis of why an intervention like antenatal syphilis screening is not being implemented. In USA a record low incidence of congenital syphilis, 20.6 cases per 100,000 live births, was recorded in 1998 by the Centers for Disease Control and Prevention (CDC) (1999a), resulting in creation of the National Plan for Syphilis Elimination (2).
Natural History of the Disease:
Syphilis is an infection of mucous membranes. Transmission of the spirochete is predominantly the result of coitus. Treponema pallidum is an elongated spiral organism, the morphology of which differs markedly from that of other bacteria. The spirochete is 5-20 microns long and approximately 0.2 microns thick. The initial response to infection with T. pallidum results in the synthesis of predominately IgM antibodies early in disease. Within two weeks antibodies of the IgG type are produced. They appear to be the prime mediator of immunity. It is probable that T. pallidum can breach the mucous membrane barrier, but it is equally probable that minute breaks in the membrane in many instances provide the true portal of infection. Treatment during incubation is almost 100% effective and should be considered mandatory in the management of persons exposed to infectious syphilis. Fortunately, of the many congenital infections, syphilis is not only the most readily prevented but also the most susceptible to therapy.
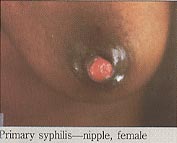
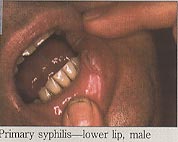
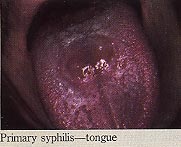
Primary Syphilis:
Primary syphilis follows an incubation period of 10 to 90 days (average 3 weeks), but usually less than 6 weeks. During pregnancy, the primary genital lesion, or sometimes multiple lesions, may be of such small size or be so located as to go unnoticed. For example, a cervical chancre is more common in pregnant women, probably because of inoculation of the friable cervix. Classical chancres are solitary lesions, painless firm ulcer with raised edges and a granular base. It persists for 2 to6 weeks and then heals spontaneously but is often accompanied by non-tender, enlarged inguinal lymph nodes. Histologic analysis reveals, the absence of secondary infection, an extensive plasma cell and lymphatic infiltration with extensive endothelial proliferation. The organism is not detected by conventional staining techniques that utilize the ability of silver salts to delineate the organism's contours or by dark-field microscopy of a wet preparation from the primary lesion.

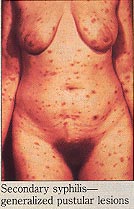
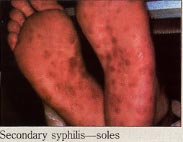
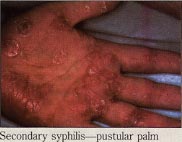
Secondary Syphilis:
The secondary stage of syphilis usually manifests 3 to 6 weeks after the primary chancre has occurred. The lesions of secondary syphilis are the consequence of; hematogenous dissemination and selective replication of treponemes at sites of slightly reduced body temperature which afford more optimal conditions for replication, i.e. skin and mucous membranes. The secondary phase is characterized by a generalized eruption, primarily on mucous membranes, the palms of the hands and the soles of the feet. Cutaneous recognizable lesions have been observed in almost every organ system. An individual, during the secondary phase of syphilis, may exhibit bone tenderness when pressure is applied. In rare instances, iritis and alopecia may occur. The cutaneous lesion of the secondary stage of syphilis is a papular lesion, except in intertriginous areas where it is condylomatous. The lesions contain large number of spirochetes and patient is capable of transmitting disease and must be regarded as highly infectious to those in the immediate environment. The small multiple lesions of the disseminated stage of acquired syphilis persist form weeks to months. If systemic immunity fails to develop, a florid type of infection called malignant secondary syphilis occurs in which the secondary lesions resemble the primary chancre. Patients with this stage of disease have high antibody titers to both specific trponemal and non-treponemal antigens and may lead to immune complex deposition in the kidneys. While the host is unable to contain the initial infection, intradermal re-challenge with T. pallidum is unlikely to induce a chancre. This situation, in which the host resists re-challenge but is unable to clear the initial infection, is called premunition.

Latency:
The third stage, latency, is a stage of disease in which systemic immunity of the host is sufficient to suppress all morphological evidence of treponemal replication. Whether subsequent disease (tertiary syphilis) develops, is a partial function not only of combined cell-mediated immunity and humoral immunity but also the virulence of organism. Secondary relapses during latency occur in 25% of untreated patients, primarily in the first year of latency. In the remaining cases, relapse occurs in the ensuing five years. The first year period is called early latency. Tertiary syphilis appears one to 20 years after the induction of latency. Gumma appears in soft tissue and viscera. While visceral involvement tends to be the rule, gumma may appear subcutaneously. The most common problem encountered is how to handle the asymptomatic patient with untreated syphilis of more than one year's duration. Lumbar puncture offers little or no additional benefits and is not cost effective in patients with symptomatic late syphilis provided that therapy is that of neuro-syphilis (3).
Congenital Syphilis (CS):
Congenital syphilis is primarily a reflection of inadequate prenatal care. Any stage of maternal syphilis may result in fetal infection. Maternal therapy given early in the infection is often adequate to eradicate spirochetal replication in the fetal tissue. The placenta, like the conceptus, is involved in the disease process. Syphilitic placentitis is manifested by a marked increase in placental weight such that the placental-fetal weight ratio is in the range of 1:3 or even 1:2. Owing to the lengthy division time of T. Pallidum compared to that of most bacteria, infection of the products of conception does not tend to result in immediate abortion. CS following hematogenous dissemination results in multiple organ involvement. T. pallidum does cross placenta and can involve fetal organ at any time during gestation; however, inflammatory lesions indicative of a host response with plasmacytoid of plasma cells do not occur until the 20th week of gestation in congenital syphilis. Wide-spread organ involvement may be responsible for a hemolytic anemia, thrombocytopenia, and hepato-spleenomegaly. These manifestations of disease may or may not be associated with cutaneous and mucous membrane lesions.
Congenital syphilis (CS) is rarely diagnosed in the neonatal period. It has become increasingly apparent that in high-risk populations, serologic surveillance at the time of delivery needs to become part of comprehensive prenatal care. An infant born to a mother whose pregnancy was complicated with syphilis will have within its intravascular compartment IgG antibody of maternal origin. These antibodies quantitatively and qualitatively may mask a fetal response to infection, which is predominantly IgM in character. The cord VDRL and FTA-ABS titers correspond to those determined for the maternal serum. If intrauterine infection has occurred, cord blood or neonatal serum will contain a composite of IgG of maternal derivation and endogenous fetal IgM. Children born of a seropositive mother must be periodically monitored for as long as 3 months for FTA-IgM antibody in order to exclude the possibility of delayed onset of infection.
Infants with congenital syphilis (CS) should have a cerebrospinal fluid (CSF) examination before treatment, since the findings will influence therapy. Penicillin is recommended and the treatment doses are discussed below. Other antibiotics are not recommended for neonatal CS. In the more severely affected new-born infants, a Herxheimer reaction often occurs in the course of penicillin therapy. Infants should be treated at birth if maternal treatment was inadequate or unknown, if drugs other than penicillin were given, or if adequate follow-up of the infant cannot be ensured.
Diagnostic Considerations and Use of Serologic Tests:
Darkfield examinations and direct fluorescent antibody tests of lesion exudate or tissue are the definitive methods for diagnosing early syphilis. A presumptive diagnosis is possible with the use of two types of serologic tests for syphilis: (a) non-treponemal (e.g., Venereal Disease Research Laboratory {VDRL} and RPR) and (b) treponemal (e.g., fluorescent treponemal antibody absorbed {FTA-ABS} and micro-hemagglutination assay for antibody to T. pallidum {MHA-TP}). The use of only one type of test is insufficient for diagnosis because false-positive non-treponemal test results occasionally occur secondary to various medical conditions. Non-treponemal test antibody titers usually correlate with disease activity, and results should be reported quantitatively. A four-fold change in titer, equivalent to a change of two dilutions (e.g., from 1:16 to 1:4 or from 1:8 to 1:32), usually is considered necessary to demonstrate a clinically significant difference between two non-treponemal test results that were obtained by using the same serologic test. It is expected that the non-treponemal test will eventually become non-reactive after treatment; however, in some patients, non-treponemal antibodies can persist at a low titer for a long period, sometimes for the remainder of their lives. This response is referred to as the serofast reaction. Most patients who have reactive treponemal tests will have reactive tests for the remainder of their lives, regardless of treatment or disease activity. However, 15%-25% of patients treated during the primary stage might revert to being serologically non-reactive after 2-3 years. Treponemal test antibody titers correlate poorly with disease activity and should not be used to assess treatment response.
Sequential serologic tests should be performed by using the same testing method (e.g., VDRL or RPR), preferably by the same laboratory. The VDRL and RPR are equally valid, but quantitative results from the two tests cannot be compared directly because RPR titers often are slightly higher than VDRL titers.
HIV-infected patients can have abnormal serologic test results (i.e., unusually high, unusually low, and fluctuating titers). For such patients with clinical syndromes suggestive of early syphilis, use of other tests (e.g., biopsy and direct microscopy) should be considered. However, for most HIV-infected patients, serologic tests appear to be accurate and reliable for the diagnosis of syphilis and for evaluation of treatment response.
No single test can be used to diagnose all cases of neuro-syphilis. The diagnosis of neuro-syphilis can be made based on various combinations of reactive serologic test results, abnormalities of cerebrospinal fluid (CSF) cell count or protein, or a reactive VDRL-CSF with or without clinical manifestations. The CSF leukocyte count usually is elevated (greater than 5 WBCs/mm3) when neuro-syphilis is present, and it also is a sensitive measure of the effectiveness of therapy. The VDRL-CSF is the standard serologic test for CSF; when reactive in the absence of substantial contamination of CSF with blood, it is considered diagnostic of neuro-syphilis. However, the VDRL-CSF may be non-reactive when neuro-syphilis is present. Some experts recommend performing an FTA-ABS test on CSF. The CSF FTA-ABS is less specific (i.e., yields more false-positive results) for neuro-syphilis than the VDRL-CSF. However, the test is believed to be highly sensitive, and some experts believe that a negative CSF FTA-ABS test excludes neuro-syphilis.
Treatment - Primary and Secondary Syphilis:
Parenteral penicillin G has been used effectively for four decades to achieve a local cure (i.e., healing of lesions and prevention of sexual transmission) and to prevent late sequelae. However, no adequately conducted comparative trials have been performed to guide the selection of an optimal penicillin regimen (i.e., the dose, duration, and preparation). Substantially fewer data are available concerning nonpenicillin regimens.
Recommended Regimen for Adults- Patients who have primary or secondary syphilis should be treated with the following regimen: Benzathine penicillin G 2.4 million units IM in a single dose (1.2 million units in each buttock).
NOTE: Recommendations for treating pregnant women and HIV-infected patients for syphilis are discussed below.
Special Considerations- Penicillin Allergy
Nonpregnant penicillin-allergic patients who have primary or secondary syphilis should be treated with one of the following regimens. Close follow-up of such patients is essential.
Recommended Regimens: Doxycycline 100 mg orally twice a day for 2 weeks, OR Tetracycline 500 mg orally four times a day for 2 weeks.
There is less clinical experience with doxycycline than with tetracycline, but compliance is likely to be better with doxycycline. Therapy for a patient who cannot tolerate either doxycycline or tetracycline should depend on whether the patient's compliance with the therapy regimen and with follow-up examinations can be ensured.
Pharmacologic and bacteriologic considerations suggest that ceftriaxone should be effective, but data concerning ceftriaxone are limited and clinical experience is insufficient to enable identification of late failures. The optimal dose and duration have not been established for ceftriaxone, but a suggested daily regimen of 1 g may be considered if treponemacidal levels in the blood can be maintained for 8-10 days. Single-dose ceftriaxone therapy is not effective for treating syphilis.
For nonpregnant patients whose compliance with therapy and follow-up can be ensured, an alternative regimen is erythromycin 500 mg orally four times a day for 2 weeks. However, erythromycin is less effective than the other recommended regimens.
Patients whose compliance with therapy or follow-up cannot be ensured should be desensitized and treated with penicillin. Skin testing for penicillin allergy may be useful in some circumstances in which the reagents and expertise to perform the test adequately is available.
The Jarisch-Herxheimer reaction is an acute febrile reaction -- often accompanied by headache, myalgia, and other symptoms that might occur within the first 24 hours after any therapy for syphilis; patients should be advised of this possible adverse reaction. The Jarisch-Herxheimer reaction often occurs among patients who have early syphilis. Antipyretics may be recommended, but no proven methods prevent this reaction. The Jarisch-Herxheimer reaction may induce early labor or cause fetal distress among pregnant women. This concern should not prevent or delay therapy.
Pregnancy:
Pregnant patients who are allergic to penicillin should be desensitized, if necessary, and treated with penicillin.
Primary or Secondary Syphilis in First and Second Trimester: Benzathine penicillin G 2.4 million units total (1.2 million in each buttock) at a single session; route of administration: IM; or Aqueous procaine penicillin G 4.8 million units total: 600,000 units daily; route of administration: IM, duration of therapy 8 days.
Primary or Secondary Syphilis in Third Trimester: Aqueous procaine penicillin G 4.8 million units total: 600,000 units daily for 8 days or Benzathine penicillin G 2.4 million units followed by 1.2 million units at each of the next 3 clinic visits, 4 days apart; route of administration: IM.
Latent Syphilis of Less Than One Year's Duration: Benzathine penicillin G 2.4 million units total at a single session; route of administration: IM; or Aqueous procaine penicillin G 4.8 million units total: 600,000 units daily for 8 days, route of administration: IM.
Latent Syphilis of Indeterminant or More Than One Year's Duration: Benzathine penicillin G 7.2 million units total: 2.4 million units weekly for 3 successive weeks; route of administration: IM; or Aqueous procaine penicillin 9 million units total: 600,000 units daily; route of administration: IM for 15 days; or Erythromycin stearate, ethysuccinate, or base (alternate drug of choice) 500 mg every 8 hours; route of administration: oral for 15 days.
Recommended Regimen for Children:
After the newborn period, children in whom syphilis is diagnosed should have a CSF examination to detect asymptomatic neuro-syphilis, and birth and maternal medical records should be reviewed to assess whether the child has congenital or acquired syphilis. Children with acquired primary or secondary syphilis should be evaluated (including consultation with child-protection services) and treated by using the following pediatric regimen.
Benzathine penicillin G 50,000 units/kg IM, up to the adult dose of 2.4 million units in a single dose.
Other Management Considerations:
All patients who have syphilis should be tested for HIV infection. In geographic areas in which the prevalence of HIV is high, patients who have primary syphilis should be retested for HIV after 3 months if the first HIV test result was negative. This recommendation will become particularly important if it can be demonstrated that intensive antiviral therapy administered soon after HIV sero-conversion is beneficial.
Patients who have syphilis and who also have symptoms or signs suggesting neurologic disease (e.g., meningitis) or ophthalmic disease (e.g., uveitis) should be evaluated fully for neuro-syphilis and syphilitic eye disease; this evaluation should include CSF analysis and ocular slit-lamp examination. Such patients should be treated appropriately according to the results of this evaluation.
Invasion of CSF by T. pallidum accompanied by CSF abnormalities is common among adults who have primary or secondary syphilis. However, neurosyphilis develops in only a few patients after treatment with the regimens described in this report. Therefore, unless clinical signs or symptoms of neurologic or ophthalmic involvement are present, lumbar puncture is not recommended for routine evaluation of patients who have primary or secondary syphilis.
Follow-Up:
Treatment failures can occur with any regimen. However, assessing response to treatment often is difficult, and no definitive criteria for cure or failure have been established. Serologic test titers may decline more slowly for patients who previously had syphilis. Patients should be reexamined clinically and serologically at both 6 months and 12 months; more frequent evaluation may be prudent if follow-up is uncertain.
Patients who have signs or symptoms that persist or recur or who have a sustained four-fold increase in non-treponemal test titer (i.e., in comparison with either the baseline titer or a subsequent result) probably failed treatment or were re-infected. These patients should be re-treated after reevaluation for HIV infection. Unless re-infection with T. pallidum is certain, a lumbar puncture also should be performed.
Failure of non-treponemal test titers to decline fourfold within 6 months after therapy for primary or secondary syphilis identifies persons at risk for treatment failure. Such persons should be reevaluated for HIV infection. Optimal management of such patients is unclear. At a minimum, these patients should have additional clinical and serologic follow-up. HIV-infected patients should be evaluated more frequently (i.e., at 3-month intervals instead of 6-month intervals). If additional follow-up cannot be ensured, re-treatment is recommended. Some experts recommend CSF examination in such situations (4).
When patients are re-treated, most experts recommend re-treatment with three weekly injections of benzathine penicillin G 2.4 million units IM, unless CSF examination indicates that neuro-syphilis is present.
Long-acting preparations of penicillin remain the treatment of choice for all stages of syphilis, regardless of HIV status. Inappropriate use of procaine-benzathine penicillin instead of benzathine penicillin G has been reported, and may result in treatment failure and complications such as neurosyphilis. Benzathine-procaine penicillin combinations and oral penicillin are not effective for the treatment of syphilis. Alternative therapies such as doxycycline are less efficacious and should only be used if there is a medical contraindication to benzathine penicillin G; close follow up is essential in these patients. Use of azithromycin as an alternative treatment for syphilis is not recommended, as evidence of resistance has emerged. (5). Rare cases of symptomatic neurosyphilis have been reported among HIV-infected men, highlighting the need for a careful neurological exam in all patients with syphilis and a syphilis test in all at-risk patients (6).
Management of Sex Partners:
Sexual transmission of T. pallidum occurs only when mucocutaneous syphilitic lesions are present; such manifestations are uncommon after the first year of infection. However, persons exposed sexually to a patient who has syphilis in any stage should be evaluated clinically and serologically according to the following recommendations:
- Persons who were exposed within the 90 days preceding the diagnosis of primary, secondary, or early latent syphilis in a sex partner might be infected even if sero-negative; therefore, such persons should be treated presumptively.
- Persons who were exposed greater than 90 days before the diagnosis of primary, secondary, or early latent syphilis in a sex partner should be treated presumptively if serologic test results are not available immediately and the opportunity for follow-up is uncertain.
- For purposes of partner notification and presumptive treatment of exposed sex partners, patients with syphilis of unknown duration who have high non-treponemal serologic test titers (i.e., greater than or equal to 1:32) may be considered as having early syphilis. However, serologic titers should not be used to differentiate early from late latent syphilis for the purpose of determining treatment.
- Long-term sex partners of patients who have late syphilis should be evaluated clinically and serologically for syphilis and treated on the basis of the findings of the evaluation.
The time periods before treatment used for identifying at-risk sex partners are (a) 3 months plus duration of symptoms for primary syphilis, (b) 6 months plus duration of symptoms for secondary syphilis, and (c) 1 year for early latent syphilis.
Treatment of latent syphilis: is intended to prevent occurrence or progression of late complications. Although clinical experience supports the effectiveness of penicillin in achieving these goals, limited evidence is available for guidance in choosing specific regimens. There is minimal evidence to support the use of non-penicillin regimens.
Recommended Regimens for Adults - The following regimens are recommended for nonallergic patients who have normal CSF examinations (if performed):
Early Latent Syphilis: Benzathine penicillin G 2.4 million units IM in a single dose.
Late Latent Syphilis or Latent Syphilis of Unknown Duration: Benzathine penicillin G 7.2 million units total, administered as three doses of 2.4 million units IM each at 1-week intervals.
Recommended Regimens for Children: After the newborn period, children in whom syphilis is diagnosed should have a CSF examination to exclude neuro-syphilis, and birth and maternal medical records should be reviewed to assess whether the child has congenital or acquired syphilis. Older children with acquired latent syphilis should be evaluated as described for adults and treated using the following pediatric regimens. These regimens are for non-allergic children who have acquired syphilis and whose results of the CSF examination were normal.
Early Latent Syphilis: Benzathine penicillin G 50,000 units/kg IM, up to the adult dose of 2.4 million units in a single dose.
Late Latent Syphilis or Latent Syphilis of Unknown Duration: Benzathine penicillin G 50,000 units/kg IM, up to the adult dose of 2.4 million units, administered as three doses at 1-week intervals (total 150,000 units/kg up to the adult total dose of 7.2 million units).
CDC Recommendations:
CDC in the United States recommends syphilis testing for all women during the early stages of pregnancy. In areas where syphilis prevalence is high or among women at high risk, testing should be done twice in the third trimester, including once at delivery. All women who deliver a stillborn infant after 20 weeks' gestation should be tested. In populations in which use of prenatal care is not optimal, CDC recommends rapid plasma reagin (RPR) card-test screening and treatment (if the RPR-card test is reactive) at the time pregnancy is determined. Syphilis screening also should be offered in emergency departments, jails, prisons, and other settings that provide episodic care to pregnant women at high risk for syphilis.
Access to and use of comprehensive prenatal care for women and adolescents who are uninsured or covered by public insurance programs (e.g., Medicaid, migrant health clinics, and the Indian Health Service) should be promoted by communities, health-care providers, and government organizations, and public awareness should be increased about the persistent risk for Congenital Syphilis (CS). Care for women with syphilis who use prenatal health services could be improved by increasing providers' adherence to screening and treatment guidelines with reminders and feedback about their prenatal syphilis screening and treatment practices. Ongoing efforts to form and maintain coalitions to develop, implement, and evaluate syphilis elimination activities and interventions also may assist in reducing the prevalence of syphilis among women of reproductive age and, in turn, eliminating CS.
Editor's Note:
Substantial progress has been made in eliminating syphilis in the United States. In 2000, the number of congenital syphilis (CS) cases was the lowest since the revised case definition was implemented in 1988, and all but two states met the national health objective for 2000. Rates in 2000 declined 51.8% since 1997, the year preceding the start of syphilis elimination efforts. Interventions designed to prevent, detect, and treat syphilis in women of reproductive age may have had a substantial role in these declines. Many of these efforts targeted the racial/ethnic minority populations with the highest CS rates and were located mostly in the South. CS elimination is feasible because of the limited numbers of cases and their highly focal distribution; however, the cornerstone of CS elimination is early detection of syphilis and treatment with penicillin, which is inexpensive, widely available, effective, and safe for the mother and fetus.
Although the concept of screening pregnant women for syphilis is simple, implementing the programs is not. In industrialized countries, despite recommendations for screening early pregnancy, stillbirths and infections in infants occur. Congenital Syphilis (CS) can be prevented, either through prevention or detection of infection in pregnant women. Programs promoting safer sex or control of sexually transmitted infection in the community will prevent maternal infection. Health policy decision-makers and program managers are key players in ensuring that a program receives adequate political, logistical and financial support.
Suggested Reading:
- World Health Organization
The Global Elimination of Congenital Syphilis: Rationale and Strategy for Action (pdf) - Centers for Disease Control and Prevention (CDC)
Congenital Syphilis - National Institutes of Health (NIH)
Congenital Syphilis
References:
- Finelli L, Berman SM, Koumans EH, Levine WC. Congenital Syphilis. Bulletin of the World Health Organization 1998;76,Suppl 2:126-128
- CDC. The national plan to eliminate syphilis from the United States. Atlanta, Georgia: US Department of Health and Human Services, CDC, National Center for HIV, STD, and TB Prevention, 1999:10-31
- Wiesel J, Rose DN, Silver AL, et al. Lumbar puncture in asymptomatic late syphilis. An analysis of the benefits and risks. Arch Intern Med 1985;145:465-468
- Walker DG, Walker GJ. Forgotten but not gone: the continuing scourge of congenital syphilis. Lancet Infectious Diseases 2002;2:432-436
- Lukehart SA, Godornes C, Molini BJ et al. Macrolide resistance in Treponema pallidum in the United States and Ireland [see comment]. N Engl J Med 2004;251(2)154-158
- CDC. Symptomatic early neurosyphilis among HIV-positive men who have sex with men-four cities, United States, January 2002-June 2004. MMWR Morb Mortal Wkly Rep 2007;56(25):625-628
Published: 5 August 2009
Dedicated to Women's and Children's Well-being and Health Care Worldwide
www.womenshealthsection.com


