Newborn Nutrition
WHEC Practice Bulletin and Clinical Management Guidelines for healthcare providers. Educational grant provided by Women's Health and Education Center (WHEC).
The landscape of breastfeeding has changed over the past several decades as more women initiate breastfeeding in the postpartum period and more hospitals are designated as Baby-Friendly Hospitals by following the evidence-based Ten Steps to Successful Breastfeeding. The number of births in such facilities has increased more than six-fold over the past decade. There are diverse and important advantages to infants, mothers, families and society for breastfeeding and the use of human milk for infant feeding. These include health, nutritional, immunologic, developmental, psychological, social, economic, and environmental benefits. Human milk feeding supports optimal growth and development of the infant while decreasing the risk of a variety of acute and chronic diseases. Healthcare providers evaluate breastfeeding infants and their mothers in the office setting frequently during the first year of life. The office setting should be conducive to providing ongoing breastfeeding support. Even mothers who are initially undecided or hesitant to breastfeed usually can do so successfully with appropriate counseling, education, and knowledgeable support, including that of a certified lactation consultant.
The purpose of this document is to review practices shown to support breastfeeding that can be implanted in the outpatient setting, with the goal of increasing the duration of exclusive breastfeeding and the continuation of any breastfeeding. Formula feeding should not be portrayed as equivalent to human milk feeding. If the mother chooses not to breastfeed after these interventions have been implemented, she should be supported in her decision.
Background
Support of successful breastfeeding begins during pregnancy. Breastfeeding has long been documented as the ideal method for feeding and promoting the optimal development of infants and children, with rare exception (1). Benefits of breastfeeding include decreased risk of lower respiratory infections, gastroenteritis, otitis media, and necrotizing enterocolitis, and later being especially important in preterm infants. Because breastfeeding is the norm for infant feeding, comparatively there are risks associated with the lack of breastfeeding, which include an increase in sudden infant death syndrome, obesity, asthma, certain childhood cancers, diabetes, and post-neonatal death (2). Breastfeeding promotes attachment and optimal cognitive development. In women lack breastfeeding is associated with an increase in the risk of breast and ovarian cancer, type 2 diabetes, heart disease, and postpartum depression (3),(4).
In the United States, The American Academy of Pediatrics (AAP) recommends exclusive breastfeeding for approximately 6 months, followed by continued breastfeeding for 1 years or longer, as mutually desired by mother and child (1). The Surgeon General's Call to Action To Support Breastfeeding in 2011 emphasized the importance of breastfeeding as a public health imperative (5). The Women's Health and Education Center (WHEC) and its partners call on its partners and members, to actively engaged in promoting and supporting breastfeeding among their patients.
Initiation of Breastfeeding
Prenatal care should include discussion of prior breastfeeding experience, feeding plans, and breast care. Ascertaiment of a history of breast surgery, trauma, or prior lactation failure is important because these situations may present special challenges to successful breastfeeding.
A healthy-newborn infant can latch on to the breast without specific assistance within the first hour after birth, and breastfeeding should be initiated within the first postnatal hour unless medically contraindicated. Appropriately triaged healthy term infants should be placed in direct skin-to-skin contact with their mothers and allowed to attempt breastfeeding immediately after birth and should remain there, with frequent assessments by hospital personnel. Care should be taken to monitor the infant's nose to avoid positions that obstruct breasting, which may lead to collapse. Skin-to-skin care should be encouraged throughout the postpartum stay, whenever possible.
Rooming-in with the mother facilitates breastfeeding. The mother should be encouraged to offer the breast whenever the infant shows early signs of hunger (e.g. increased alertness, increased physical activity, mouthing, or rooting), not to wait until the infant cries. When awake, the newborn infant should be encouraged to feed frequently (8-12 breastfeedings every 24 hours) until safely to help stimulate milk production. Scheduling specific times for feeding is not encouraged. In the early weeks after birth, an infant may need to be aroused to feed if 4 hours have elapsed since the last nursing. This is especially true for a late-preterm infant. Usually, it is practical to alternate the breast used to initiate the feeding and equalize the time spent at each breast over the day.
Supplemental feedings including water, glucose water, formula, and other fluids should not be given to the breastfeeding infant unless ordered by the healthcare provider after documentation of a medical indication. Intermittent bottle-feeding of a breastfed newborn infant may lessen the success of breastfeeding (6). If the infant's appetite is partially satisfied by supplements, the infant will take less from the breast, and milk production will be diminished.
Epidemiology
The rate of initiation of any breastfeeding in the US population is 81.1%, as surveyed in 2016 (7). Although the rate of breastfeeding initiation approaches the Healthy People 2020 target of 81.9%, only 22.3% of US infants are breastfed at age 6 months (8). There are significant disparities in terms of breastfeeding rates in the country; among black infants, only 66.3% are breastfed at all, and only 14.6% are exclusively breastfed through the first 6 months of life. Among Native American and Alaska Native infants, breastfeeding initiation is 68.3% and exclusive breastfeeding rates at 6 months are 17.9%. Mothers are more likely to breastfeed if they are married, have a college education, live in metropolitan areas, do not experience poverty, and do not receive benefits from Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). WIC provides targeted breastfeeding support and peer-counseling services for mothers who qualify for their services. Infants most likely to experience toxic stress are least likely to be breastfed. According to the 2005-2007 Infant Feeding Practices Study II, 85% of US mothers intended to breastfeed exclusively for >3 months; however, only 32.4% achieved their intended exclusive breastfeeding duration (9).
The Ten Steps to Successful Breastfeeding
There is no doubt regarding the multiple benefits of breastfeeding for infants and society in general. Therefore, the World Health Organization (WHO) in conjoint effort with United Nations International Children's Emergency Fund (UNICEF) developed the "Ten Steps to Successful Breastfeeding" in 1992, which became the backbone of the Baby Friendly Hospital Initiative (BFHI). Following this development, many hospitals and countries intensified their position towards creating a "breastfeeding oriented" practice (10). Over the past two decades, the interest increased in the BFHI and the Ten Steps. However, alongside the implementation of the initiative, extensive research continues to evaluate the benefits and dangers of the suggested practices. Hence, it is our intention to make a critical evaluation of the current BFHI and the Ten Steps recommendations in consideration of the importance of providing an evidence-based breastfeeding supported environment for our mothers and infants.
- Have a written breastfeeding-friendly policy that is routinely communicated to all health care staff.
- Train all health care staff in the skills necessary to implement this policy.
- Inform all pregnant women about the benefits and management of breastfeeding.
- Help mothers initiate breastfeeding within 1 hour of birth.
- Show mothers how to breastfeed and how to maintain lactation, even if they are separated from their infants.
- Give infants no food or drink other than breast milk, unless medically indicated.
- Practice rooming in: allow mothers and infants to remain together 24 hours a day.
- Encourage breastfeeding on demand.
- Give no pacifiers or artificial nipples to breastfeeding infants.
- Foster the establishment of breastfeeding support groups and refer mothers to them on discharge from the hospital or birth center.
For the national breastfeeding targets to be met, outpatient support from pediatricians and other health care providers is imperative. As more infants are being discharged from hospitals designated as Baby-Friendly and having successfully initiated breastfeeding, it is essential that the pediatricians with whom they will follow up are knowledgeable about breastfeeding and that their office practices are prepared to support these breastfeeding practices and policies. A pediatrician or other knowledgeable and experienced health care professional should see the newborn infant at 3-5 days of age or within 48 hours of discharge. A secondary appointment should be scheduled when infant is 2-3 weeks of age to monitor progress.
Monitoring Breastfeed Newborn
Tracking an infant's weight provides a useful assessment of adequacy of breast milk intake. Weight can be plotted on hour-specific curves for vaginal or cesarean delivery to assist with determining when a term infant requires a careful evaluation of the feeding techniques being used and the adequacy of breastfeeding (11).
Excessive or prolonged infant weight loss should prompt a thorough evaluation by the pediatric care provider. Close monitoring of the infant and consideration of supplementation with infant formula should be considered. Although previous literature suggested that a failure to regain birth weight by 10 days required further evaluation, a very large population-based study found that only about one half of infants had regained their birth weight on the appropriate graph can provide guidance on the need for further evaluation (12),(13). Although delayed onset of lactogenesis is relatively common, true failure of lactogenesis occurs far less frequently, and with support, breastfeeding occurs far less frequently, and with support, breastfeeding can usually be established. Exclusive breastfeeding is the ideal nutrition and is almost always sufficient to support optimal growth and development for the healthy term infant for approximately 6 months after delivery. In families with a strong history of allergy, breastfeeding is likely to be especially beneficial. Infants weaned before the age of 12 months should not receive cow's milk feeding; instead, they should receive iron-fortified infant formula.
Contraindication to Breastfeeding
Contraindications to breastfeeding include certain maternal infectious diseases and medications. A mother with active herpes simplex virus infection may breastfeed her infant if she has no vesicular lesions in the breast area, if she observes careful hand hygiene. A mother who has herpes simplex lesions on a breast should not breastfeed her infant on that breast until the lesions are cleared. Endometritis and mastitis that is being treated with antibiotics is not a contraindication to breastfeeding.
The situations that are not in the best interest of the infant for breastfeeding are: newborn infant with classic galactosemia (who must be fed non-lactose-based formula), the newborn infant whose mother is positive for human T-cell lymphotrophic virus type I or II, and the newborn infant whose mother uses non-medical drugs. In situations where maternal breast milk confers specific medical advantages (i.e. very-low-birth-weight infants), the clinician must weigh the risks and benefits of formula versus maternal milk, which may be contaminated by non-medical drugs (e.g. tetrahydrocannabinol). In the US and other developed countries where formula is safe and readily available, women infected with HIV should not breastfeed their infants. Mothers who receive certain radioactive materials should not breastfeed if there is radioactivity in the milk, and mothers who are receiving antimetabolites or chemotherapy should not breastfeed until the medication has cleared from the milk. Rarely, a specific vaccine, such as live-attenuated rabies, is contraindicated during breastfeeding. Please visit the guidelines stated by the Center for Disease Control and Prevention (CDC) for updated information (15).
Breast milk provides protections against many respiratory diseases, including influenza (flu). A mother with suspected or confirmed flu should take all possible precautions to avoid spreading the virus to her infant while continuing to provide breast milk to her infant. Flu is not spread to infants through breast milk (16). When an infant has flu, the mother should be encouraged to continue breastfeeding or feeding expressed breast milk to her infant. Flu vaccination is safe for breastfeeding women and their infants aged 6 months and older.
Human Milk Storage
There are many situations in which a mother might be separated from her infant, necessitating her to express and store her breast milk. A mother who is in school or employed outside of the home can maintain exclusive human milk feeding by providing expressed milk to be given in her absence; therefore, it is important to encourage and support mothers in providing their infants with expressed milk. All mothers who provide milk for their infants should be instructed in the proper techniques of milk collection and storage to minimize bacterial contamination. Careful hand hygiene is critical before handling the breast, the equipment, or the milk. Previous practices of washing the breast and discarding the first expressed milk did not result in a decrease in bacterial colonization of milk, and therefore, are not necessary (17). Although manual expression, when performed correctly, yields relatively uncontaminated milk, many women prefer to use a breast pump. All parts of the pump that are in contact with the milk should be washed carefully with hot, soapy water, and rinsed and dried thoroughly after each use.
The Academy of Breastfeeding Medicine recommends that fresh expressed milk be stored in sterile glass or plastic containers or plastic bags that are free of bisphenol A and made specifically for human milk storage. According to the Academy of Breastfeeding Medicine, milk that is refrigerated (at or below 4oC [39oF]) should optimally be used within 72 hours, although 5-8 days is acceptable under very clean conditions (18). Frozen milk should optimally be stored for up to 6 months, although 12 months is acceptable.
Breast Milk Storage Guidelines
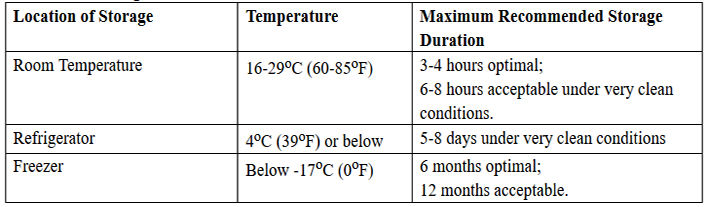
Human milk should not be defrosted in extremely hot water or in a microwave oven. The very high temperatures that may be reached with these methods can destroy valuable components of the milk and may result in thermal injury to the infant. Previously frozen milk thawed for 24-hours should not be left at room temperatures for more than a few hours because of its reduced ability to inhibit bacterial growth. Whether thawed breast milk can be safely frozen is uncertain. When using human milk in neonatal care units, it is essential to have policies and procedures for storing in milk, appropriately identifying the milk, and checking the milk before giving it to an infant.
Infant Outcomes
To date, the most comprehensive publication that reviews and analyzes the published scientific literature that compares breastfeeding and commercial infant formula feeding as to health outcomes is the report prepared by the Evidence-based Practice Centers of the Agency for Healthcare Research and Quality (AHRQ) of the US Department of Health and Human Services titled: Breastfeeding and Maternal and Infant Health Outcomes in Developed Countries (19). The following analysis summarize and update AHRQ meta-analyses and provide and expanded analysis regarding health outcomes:
Respiratory Tract Infections and Otitis Media
The risk of hospitalization for lower respiratory tract infections in the first year is reduced 72% if infants are breastfed exclusively for more than 4 months (20), infants who exclusively breastfed for 4-6 months had a four-fold increase in the risk of pneumonia compared with infants who exclusively breastfed for more than 6 months (20). The severity (duration of hospitalization and oxygen requirements) of respiratory syncytial virus bronchiolitis is reduced by 74% in infants who breastfed exclusively for 4 months compared with infants who never or only partially breastfed.
Any breastfeeding compared with exclusive commercial infant formula feeding will reduce the incidence of otitis media by 23% (21). Exclusive breastfeeding for more than 3 moths reduces the risk of otitis media by 50%. Serious colds and ear and throat infections were reduced by 63% in infants who exclusively breastfed for 6 months (21).
Gastrointestinal Tract Infections and Necrotizing Enterocolitis
Any breastfeeding is associated with a 64% reduction in the incidence of non-specific gastrointestinal tract infections, and this effect lasts for 2 months after cessation of breastfeeding (21),(22). Meta-analyses of four randomized clinical trials performed over the period 1983 to 2005 support the conclusion that feeding preterm infants human milk is associated with a significant reduction (58%) in the incidence of necrotizing enterocolitis (22).
Sudden Infant Death Syndrome (SIDS) and Infant Mortality
Meta-analyses with a clear definition of degree of breastfeeding and adjusted for cofounders and other known risks for sudden infant death syndrome (SIDS) note that breastfeeding is associated with a 36% reduced risk of SIDS. A proportion (21%) of the US infant mortality has been attributed, in part, to the increased rate of SIDS in infants who were never breastfed (23). That the positive effect of breastfeeding on SIDS rate is independent of sleep position was confirmed in a large case-control study of supine-sleeping infant.
It has been calculated that more than 900 infant lives per year may be saved in the United States if 90% of mothers exclusively breastfed for 6 months. In the 42 developing countries in which 90% of the world's childhood deaths occur, exclusive breastfeeding for 6 months and weaning after 1 year is the most effective intervention, with the potential of preventing more than 1 million infant deaths per year, equal to preventing 13% of the world's childhood mortality (24).
Allergic Disease
There is protective effect of exclusive breastfeeding for 3 to 4 months in reducing the incidence of clinical asthma, atopic dermatitis, and eczema by 27% in a low-risk population and up to 42% in infants with positive family history (25). There are conflicting studies that examine the timing of adding complementary foods after 4 months and the risk of allergy, including food allergies, atopic dermatitis, and convincing data that delaying introduction of potentially allergenic foods after 6 months has any protective effect (25). One problem in analyzing this research is the low prevalence of exclusive breastfeeding at 6 months in the study populations. Thus, research outcomes in studies that examine the development of atopy and the timing of introducing solid foods in partially breastfed infants may not be applicable to exclusively breastfed infants.
Celiac Disease and Inflammatory Bowel Disease
There is reduction of 52% in the risk of developing celiac disease in infants who were breastfed at the time of gluten exposure (26). Overall, there is an association between increased duration of breastfeeding and reduced risk of celiac disease when measured as the presence of celiac antibodies. The critical protective factor appears to be not the timing of the gluten exposure but the overlap of breastfeeding at the time of the initial gluten ingestion. Thus, gluten-containing foods should be introduced while the infant is receiving only breast milk and not infant formula or other bovine milk products.
Breastfeeding associated with a 31% reduction in the risk of childhood inflammatory bowel disease (26). The protective effect is hypothesized to result from the interaction of the immunomodulating effect of human milk and the underlying genetic susceptibility of the infant. Different patterns of intestinal colonization in breastfed versus commercial infant formula-fed infants may add to the preventive effect of human milk.
Obesity
Because rates of obesity are significantly lower in the breastfed infants, national campaigns to prevent obesity begin with breastfeeding support (27). Although complex factors confound studies of obesity, there is a 15% to 30% reduction in adolescent and adult obesity rates if any breastfeeding occurred in infancy compared with no breastfeeding (27). The duration of breastfeeding also is inversely related to the risk of overweight; each month of breastfeeding being associated with a 4% reduction in risk (27). This is of importance, because breastfed infants self-regulate intake volume irrespective of maneuvers that increase available milk volume, and the early programming of self-regulation, in turn, affects adult weight gain. This concept is further supported by the observations that infants who are fed by bottle, formula, or expressed breast milk will have increased bottle emptying, poorer self-regulation, and excessive weight gain in late infancy (older than 6 months) compared with infants who only nurse from the breast.
Diabetes
Up to a 30% reduction in the incidence of type 1 diabetes mellitus is reported for infants who exclusively breastfed for at least 3 months, thus avoiding exposure to cow milk protein (28). It has been postulated that the presumed mechanism in the development of type I diabetes mellitus is the infant's exposure to cow-milk β-lactoglobulin, which stimulates an immune-mediated process cross-reacting with pancreatic β cells. A reduction of 40% in the incidence of type 2 diabetes mellitus is reported, possibly reflecting the long-term positive effect of breastfeeding on weight control and feeding self-regulation.
Childhood Leukemia and Lymphoma
There is a reduction in leukemia that is correlated with the duration of breastfeeding (28). A reduction of 20% in the risk of acute lymphocytic leukemia and 15% in the risk of acute myeloid leukemia in infants breastfed for 6 months or longer (29). Breastfeeding for less than 6 months is protective but of less magnitude (approximately 12% and 10%, respectively). The question of whether the protective effect of breastfeeding is a direct mechanism of human milk on malignancies or secondarily mediated by its reduction of early childhood infections has yet to be answered.
Neurodevelopment Outcomes
Consistent differences in neurodevelopmental outcome between breastfed and commercial infant formula-fed infants have been reported, but the outcomes are confounded by differences in parental education, intelligence, home environment, and socioeconomic status (30). The large, randomized Promotion of Breastfeeding Intervention Trial provided evidence that adjusted outcomes of intelligence scores and teacher's ratings are significantly greater in breastfed infants (30). In addition, higher intelligence scores are noted in infants who exclusively breastfed for 3 months or longer, and higher teacher ratings were observed if exclusive breastfeeding was practiced for 3 months or longer. Significantly positive effects of human milk feeding on long-term neurodevelopment are observed in preterm infants, the population more at risk for these neurodevelopmental outcomes.
Donor Human Milk, Pasteurization and Distribution
The use of donor human milk is increasing for high-risk infants, primarily for infants born weighing <1,500 g or those who have severe intestinal disorders. Pasteurized donor milk may be considered in situations in which the supply of maternal milk is insufficient. The use of pasteurized donor milk is safe when appropriate measures are used to screen donors and collect, store, and pasteurize the milk and then distribute it through established human milk banks. The use of non-pasteurized donor milk and other forms of direct, Internet-based, or informal human milk sharing does not involve this level of safety and is not recommended. It is important that health care providers counsel families considering milk sharing about the risks of bacterial or viral contamination of non-pasteurized human milk and about the possibilities of exposure to medications, drugs, or herbs in human milk (31).
Currently, the use of pasteurized donor milk is limited by its availability and affordability. The development of public policy to improve and expand access to pasteurized donor milk, including policies that support improved governmental and private financial support for donor milk banks and the use of human milk, is important. Donor milk banks represent safe and effective approach to obtaining, pasteurizing, and dispensing human milk for use in neonatal intensive care units (NICUs) and other settings. However, accessibility to donor milk in the United States continues to be substantially limited in terms of supply, cost, and distribution.
The number of human milk banks in the United States is increasing. Currently, there are 20 donor milk banks in the United States and 4 in Canada that pasteurize milk as part of a professional organization for supporters of non-profit human milk banking, the Human Milk Banking Association of North America (HMBANA); 7 others are in various stages of planning and development. HMBANA has established policies for donor milk collection, as do commercial human milk banks (32).
Pasteurization
Several methods may be used to pasteurize donor human milk, and these have been reviewed extensively. The Holder pasteurization method uses heating at 62.5oC for 30 minutes and is the primarily method used by HMBANA milk banks (32). One commercial milk bank, Medolac Laboratories (Lake Oswego, OR), uses a different thermal pasteurization system.
Distribution
In the United States and Canada, most donor milk is distributed by established milk banks to NICUs. Each milk bank and/or processing center has policies, including cost-related guidelines, for this distribution. The distribution of donor milk may be subject to federal or state guidelines in some situations. Frozen donor human milk is distributed by using shipping guidelines established by the milk banks. Receiving hospitals are provided guidance related to temperature and other storage conditions for milk, and these may be subject to state and local regulations. Hospitals that use frozen donor human milk must have properly regulated freezers and other methods for handling and tracking donor milk.
Safety
Human milk is a biological product; therefore, whether from an infant's own mother of a donor mother, there will always be concerns about contamination. Possible contaminants are infectious agents, including both bacteria and viruses, and contamination with other substances, most notably toxic components in the environment (e.g. pesticides, mercury, medications, drugs, or herbs).
The process of pasteurization destroys cells, such as neutrophils and stem cells, and affects macronutrients and anti-inflammatory factors. In addition, pasteurization can eliminate bacterial strains with probiotic properties. Substantial evidence describing these losses is available (33). Bioactive components of human milk, including lactoferrin and immunoglobulins, are substantially decreased by pasteurization, but there is much less effect on macro- and micronutrients, including vitamins (33). Overall, the benefits of improved feeding tolerance and clinical outcomes support the concept that some nutrient losses of bioactive components should not limit the use of donor milk or preclude its pasteurization before use.
Pacifier Use
Given the documentation that early use of pacifiers may be associated with less successful breastfeeding, pacifier use in the neonatal period should be limited to specific medical situations (34). These include uses for pain relief, as a calming agent, or as part of structured program for enhancing oral motor function. Because pacifier use has been associated with a reduction in SIDS incidence, mothers of healthy term infants should be instructed to use pacifiers at infant nap or sleep time after breastfeeding is well established, at approximately 3 to 4 weeks of age (34).
Vitamins and Mineral Supplements
Intramuscular vitamin K1 (phytonadione) at a dose of 0.5 to 1.0 mg should routinely be administered to all infants on the first day to reduce the risk of hemorrhagic disease of newborn (35). A delay of administration until after the first feeding at the breast but not later than 6 hours of age is recommended. A single oral dose of vitamin K should not be used, because oral dose is variably absorbed and does not provide adequate concentrations or stores for breastfed infant (35).
Vitamin D deficiency/insufficiency and rickets has increased in all infants because of decreased sunlight exposure secondary to changes in lifestyle, dress habits, and use of topical sunscreen preparations. To maintain an adequate serum vitamin D concentration, all breastfed infants routinely should receive an oral supplement of vitamin D 400 U per day, beginning at hospital discharge (36).
Supplementary fluoride should not be provided during the first 6 months. From age 6 months to 3 years, fluoride supplementation should be limited to infants residing in communities where the fluoride concentration in water is <0.3 ppm (37). Complementary food rich in iron and zinc should be introduced at about 6 months of age. Supplementation of oral iron drops before 6 months may be needed to support iron stores.
Premature infants should receive both a multivitamin preparation and an oral iron supplement until they are ingesting a completely mixed diet and their growth and hematologic status are normalized.
Recommendations Regarding Consumption of Raw or Unpasteurized Milk and Milk Products
Foodborne illness accounts for substantial morbidity and mortality in the United States. Estimates suggest that each year, as many as 48 million Americans experience foodborne illness, accounting for 128,000 hospitalizations and 3,000 deaths (38). Among the most preventable of these foodborne illnesses are infections related to ingestion of raw or unpasteurized milk and milk products, because of ubiquitous access to healthy, pasteurized milk and milk products, as well as legislation prohibiting the sale of raw dairy products in much of the United States. Pasteurization of milk in the United States began in 1920s. although most milk and milk products consumed today in the United States are pasteurized, an estimated 1% to 3% of all dairy products consumed in the United States are not pasteurized (39).
Sales of raw or unpasteurized milk and milk products are still legal in at least 30 states in the United States. Raw milk and milk products from cows, goats, and sheep continue to be a source of bacterial infections attributable to several virulent pathogens, including Listeria monocytogenes, Campylobacter jejuni, Salmonella species, Brucella species, and Escherichia coli. These infections can occur in both healthy and immunocompromised individuals, including older adults, infants, young children, and pregnant women and their unborn fetuses, in whom life-threatening infections and fetal miscarriage can occur. Efforts to limit the sale of raw milk products have met with opposition from those who are proponents of the purported health benefits of consuming raw milk products, which contain natural or unprocessed factors not inactivated by pasteurization. However, the benefits of these natural factors have not been clearly demonstrated in evidence-based studies, and therefore, do not outweigh the risks of raw milk consumption (40). Substantial data suggest that pasteurized milk confers equivalent health benefits compared with raw milk, without additional risk of bacterial infections.
The Women's Health and Education Center (WHEC) strongly supports the national and international associations in endorsing the consumption of only pasteurized milk and milk products for pregnant women, infants and children. WHEC also endorses a ban on the sale of raw or unpasteurized milk and milk products throughout the United States, including the sale of certain raw milk cheeses, such as fresh cheeses, soft cheeses, and soft-ripened cheeses. This recommendation is based on the multiplicity of data regarding the burden of illness associated with consumption of raw and unpasteurized milk and milk products, especially among pregnant women, fetuses and newborn infants, and infants and young children, as well as strong scientific evidence that pasteurization does not alter the nutritional value of milk.
Summary
Research and practice in the last two decades have reinforced the conclusion that breastfeeding and use of human milk confer unique nutritional and non-nutritional benefits to the infant and the mother, and in turn, optimize infant, child, and adult health as well as child growth and development. Recently, published evidence-based studies have confirmed and quantitated the risk of not breastfeeding. Thus, infant feeding should not be considered as a lifestyle choice but rather as a basic health issue. As such, the healthcare provider's role in advocating and supporting proper breastfeeding practices is essential and vital for the achievement of this preferred public health goal.
The Maternal and Child Health Bureau of the US Department of Health and Human Services, with support from the Office of Women's Health, has created a program, "The Business Case for Breastfeeding," that provides details of economic benefits to the employer and toolkits for the creation of such programs. The Patient Protection and Affordable Care Act passed by Congress in March 2010 mandates that employers provide "reasonable break time" for nursing mothers and private non-bathroom areas to express breast milk during their workday. The establishment of these initiatives as the standard workplace environment will support mothers in their goal of supplying only breast milk to their infants beyond the immediate postpartum period.
References
- Eidelman AI, Schanler RJ, Johnston M, et al. Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 2012;129(3). Available at: http://pediatrics.aappublications.org/content/129/3/e827.full Retrieved on 22 March 2018
- Grummer-Strawn LM, Rollins N. Summarizing the health effects of breastfeeding. Acta Paediatr 2015;104(467):1-2
- Collaborative Group on Hormonal Factors in Breast Cancer. Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50,302 women with breast cancer and 96,973 women without the disease. Lancet 2002;360(9328):187-195
- Stuebe AM, Rich-Edwards JW, Willett WC, et al. Duration of lactation and incidence of type 2 diabetes. JAMA 2005;294(20):2601-2610
- US Department of Health and Human Services. The Surgeon General's Call to Action To Support Breastfeeding. Washington, D.C.: US Department of Health and Human Services, Office of the Surgeon General; 2011. Available at: https://www.surgeongeneral.gov/library/calls/breastfeeding/ Retrieved on 28 March 2018
- Breastfeeding in underserved women: increasing initiation and continuation of breastfeeding. Committee Opinion No. 570. American College of Obstetricians and Gynecologists. Obstet Gynecol 2013;122:423-428
- Centers for Disease Control and Prevention. National immunization survey. Available at: http://www.cdc.gov/breastfeeding/data/nis_data/rates-any-exclusive-bf-socio-dem-2013.htm Retrieved on 26 February 2018
- US Department of Health and Human Services. Healthy People 2020: maternal, infant, and child health. August 2016
- Perrine CG, Scanlon KA, Li R, et al. Baby-friendly hospital practices and meeting exclusive breastfeeding intention. Pediatrics 2012;130(1):54-60
- Gomez-Pomar E, Blubaugh R. The baby friendly hospital initiative and the ten steps for successful breastfeeding: a critical review of literature. J Perinatol 2018; Feb 7. doi: 101038/s41372-018-0068-0. [Epub ahead of print]
- Penn State Hershey Medical Center. Newborn weight tool. Available at: https://www.newbornweight.org/ Retrieved on 28 February 2018
- Flaherman VJ, Schaefer EW, Kuziewicz MW, et al. Early weight loss nomograms for exclusively breastfed newborns. Pediatrics 2015;135:e16-23
- Miller JR, Flaherman VJ, Schaefer EW, et al. Early weight loss nomograms for formula fed newborns. Hosp Pediatr 2015;5(5):263-268
- Lawrence RA, Lawrence R. Breastfeeding: A guide for the medical profession. 2016; 8th edition
- Centers for Disease Control and Prevention. Breastfeeding and Vaccinations. Available at: https://www.cdc.gov/breastfeeding/recommendations/vaccinations.htm Retrieved on 1 March 2018
- Rasmussen SA, Kissin DA, Yeung LF, et al. Preparing for influenza after 2009 HINI: Special Considerations for Pregnant Women and Newborns. Am J Obstet Gynecol 2011;204:S13-20
- Reyes-Foster BM, Carter SK, Hinojosa MS. Human milk handling and storage practices among peer milk-sharing mothers. J Hum Lact 2017;33:173-180
- Academy of Breastfeeding Medicine Protocol Committee. Breast milk storage guidelines. Breastfeed Med 2011;6:159
- Ip S, Chung M, Raman G, et al. Tufts-New England Medical Center Evidence-based Practice Center, Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Report). 2007;153:1-186
- Nishimura T, Suzue J, Kaji H. Breastfeeding reduces the severity of respiratory syncytial virus infection among young infants: a multi-center prospective study. Pediatr Int 2009;51:812-816
- Duijts L, Jaddoe VW, Hofman A, Moll HA. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics 2010;126:1-3
- Sullivan S, Schanler RJ, Kim JH, et al. an exclusively human milk-based diet is associated with a lower rate of necrotizing enterocolitis than a diet of human milk and bovine milk-based products. J Pediatr2010;156:562-567
- Task Force on Sudden Infant Death Syndrome. SIDS and other sleep-related infant deaths: expansion of recommendations for a safe infant sleeping environment. Pediatrics 2011;128:1030-1039
- Jones G, Steketee RW, Black RE, et al. Bellagio Child Study Group. How many child deaths can we prevent this year? Lancet 2003;362:65-71
- Nwaru BI, Erkkola M, Ahonen S, et al. Age at the introduction of solid foods during the first year and allergic sensitization at age 5 years. Pediatrics 2010;125:50-59
- Barclay AR, Russell RK, Wilson ML, et al. Systematic review: the role of breastfeeding in the development of pediatric inflammatory bowel disease. J Pediatr 2009;155:421-426
- Li R, Fein SB, Grummer-Strawn LM. Association of breastfeeding intensity and bottle-emptying behaviors at early infancy with infants' risk for excess weight at late infancy. Pediatrics 2008;122:S77-S84
- Rsenbauer J, Herzig P, Giani G. Early infant feeding and risk of type 1 diabetes mellitus: a nationwide population-based case-control study in pre-school children. Diabetes Metab Res Rev 2008;24:211-222
- Rudant J, Orsi L, Menegaux F, et al. Childhood acute leukemia, early common infections, and allergy: The ESCALE Study. Am J Epidimiol 2010;172:1015-1027
- Isaacs EB, Fishl BR, Quinn BT, et al. Impact of breast milk on intelligence quotient, brain size, and white matter development. Pediatr Res 2010;67:357-362
- Palmquist AE, Doehler K. Human milk sharing practices in the U.S. Matern Child Nutr 2016;12:278-290
- Human Milk Banking Association of North America. Donor Human Milk Processing; available at: https://www.hmbana.org/milk-processing Retrieved on 28 February 2018
- Coscia A, Peila C, Bertino E, et al. Effect of Holder pasteurization on human milk glycosaminoglycans. J Pediatr Gastroenterol Nutr 2015;60:127-130
- O'Connor NR, Tanabe KO, Siadaty MS, et al. Pacifiers and breastfeeding: a systematic review. Arch Pediatr Adolesc Med 2009;163:378-382
- American Academy of Pediatrics Committee on Fetus and Newborn. Controversies concerning vitamin K and the newborn. Pediatrics 2003;112:191-192
- Wagner CL, Greer FR, American Academy of Pediatrics Section on Breastfeeding, American Academy of Pediatrics Committee on Nutrition. Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics 2008;122:1142-1152
- American Academy of Pediatric Dentistry. Guidelines for Fluoride, Revised 2014. Available at: http://www.aapd.org/media/Policies_Guidelines/P_FluorideUse.pdf Retrieved 7 March 2018
- Centers for Disease Control and Prevention. Estimates of foodborne illness in the United States. Available at: https://www.cdc.gov/foodborneburden/ Retrieved on 9 March 2018
- Langer AJ, Ayers T, Grass J, et al. Centers for Disease Control and Prevention. Non-pasteurized dairy products, disease outbreaks, and state laws-United States, 1993-2006. Emrg Infect Dis 2012:18:385-391
- American Academy of Pediatrics. Prevention of disease from potentially contaminated food products. In: Pickering LK, Baker CJ, Kimberlin DW, Long SS, eds. Red Book: 2012 Report of the Committee on Infectious Diseases. 28th ed. Elk Grove Village, IL; American Academy of Pediatrics; 2012; 917-918
Published: 20 June 2018
Dedicated to Women's and Children's Well-being and Health Care Worldwide
www.womenshealthsection.com


