Update on Colposcopic TerminologyWHEC Practice Bulletin and Clinical Management Guidelines for healthcare providers. Educational grant provided by Women's Health and Education Center (WHEC). Since its description in 1925, colposcopy has served as a tool that has helped in saving the lives of many women with cervical precancer and cancer. To describe and interpret the colposcopic findings, colposcopists use the terminology of the International Federation of Cervical Pathology and Colposcopy (IFCPC). The current nomenclature committee was established at the 2008 International Federation of Cervical Pathology and Colposcopy World Congress in Auckland, New Zealand. The committee examined the past three International Federation of Cervical Pathology and Colposcopy terminologies from 1975, 1990 and 2002 by reviewing publications that critically analyzed each colposcopic sign, aiming to create an evidence-based terminology (1). In United States, the numbers of cases of cervical cancer diagnosed each year has been stable for over a decade at approximately 11,000; the numbers of deaths each year number just around 4,000 (2). These numbers remain stable despite population growth and the rapid rise in the incidence of pre-invasive disease since the 1960s, coincident with the increase in number of sexual partners and earlier age of onset of sexual relations in the general population. It is important to note that over half of the women diagnosed with and dying from cervical cancer have never undergone cytologic screening, or have been adequately screened. Older women, socio-economically disadvantaged women, and recent immigrants to the United States from underdeveloped countries are at highest risk for lack of adequate screening. Over the past three decades, we have come to understand that human papillomas viruses (HPVs) are present in essentially all true cervical neoplasia, explaining the epidemiology of the disease. Of the more than 100 types of HPVs approximately 40 may involve the anogenital tract. Approximately 15 HPV types are considered oncogenic, causing virtually all cases of cervical cancer. HPV 16 alone accounts for over 50% of cancers and HPV 18 is responsible for an additional 10-15% (3). Identified risk factors for cervical cancer such as early age at first intercourse and multiple sexual partners are proxies for risk of HPV infection. However, HPV infection is very common and cervical cancer is not. Co-factors such as smoking, high parity, and host immune responses also play a role. The purpose of this document is review new colposcopy terminology and its implementation for diagnosis, treatment, and research. This document has been expanded to include terminology of both cervix and vagina. Various human papillomas virus (HPV) lesions and intraepithelial neoplasia may occur in the vagina as a primary lesion or in continuum with cervical intraepithelial neoplasia. Although a transformation zone may occur, for example in diethylstilbestrol (DES) exposed patients, where islands of columnar epithelium may be found within the squamous epithelium (adenosis), the cervical transformation zone types are irrelevant in the vagina. As the representative body of the national societies of colposcopy and cervical pathology, the IFCPC recommends that the 2011 terminology replace all other terminologies and be implemented without delay for diagnosis, treatment and research. Colposcopy: The Colposcope and InstrumentationIntroductionThe purpose of colposcopy is the examination of the uterine cervix and lower genital tract epithelium under magnification, identification of potentially dysplastic or cancerous areas, and performance of directed biopsies of abnormal areas to provide a histological diagnosis. Dr. Hans Hinselmann performed the first colposcopic examination by mounting lenses on a pile of books and placing an ordinary lamp above his head. The first true colposcope he developed was a fixed binocular instrument that was mounted on a tripod and equipped with a light source, with a mirror to direct the light. Since that time, a wide variety of advances have been made that improve the functioning and capabilities of the colposcope. The Modern ColposcopeA colposcope is typically defined as a stereoscopic binocular field microscope with a long focal length and powerful light source. Video colposcopes and optical colposcopes with video feed allow patient and student teaching and facilitate digital image capture. Today, colposcopes permit magnification between x2 and x40, although most routine colposcopic work can be accomplished at x10 to x15 magnifications (4). Some scopes have a single fixed magnification level. Others have a series of par-focal lenses or a smooth zoom capability that allows for easy adjustment of the magnification via knob or rotor. Lower magnification yields a wider view and a greater depth of field for observation. Higher magnification can reveal small features such as abnormal blood vessel patterns and other finer details. As the magnification level increases, the field of view and illumination levels usually decrease. Interchangeable eyepieces with various levels of magnification are available for most colposcopes. Changing the magnification of the eyepieces alters the magnification levels achieved by the scope. Some eyepieces can be individually adjusted to compensate for variance in individual user's vision. A diopter scale on the side of the eyepiece can identify these. Eyepieces can be adjusted in a manner similar to microscopes to adjust to each colposcopist's interpupillary distance. Eyepiece hoods or collars can be extended, or can be folded back or removed if the colposcopist wears glasses during the examination. Changing the power of the objective lenses also alters the magnification and working distance (space between the head of the scope and the focal point) of the scope. The usual working distance (focal length) of a colposcope is 30 cm. The shorter the focal length, the closer the head of the scope must be to the introitus for clear focus, making it harder to use instruments while viewing through the scope. This also makes it more difficult to work in the vagina with the scope in place. Longer focal lengths may be uncomfortable for colposcopists with shorter arms. Grossly moving the head of the scope forward or backward coarsely focuses most standard scopes. This can be accomplished by physically lifting and moving the scope, rocking or tilting the scope on a stationary base, rolling it on casters, or pivoting the supporting arm. Most scopes also have a fine focus handle that is attached to a machine screw under the mounting bracket for the colposcope head. Applying pressure to this handle can be used to subtly control the alignment of the scope, and twisting it produces very gradual forward or backward movements of the head for exquisite fine focus control. A flexible articulating swivel arm or overhead boom type colposcope can be mounted on a stable base (with or without wheels), the wall, or an examination table. A column- or stick-mounted scope can easily be moved from place to place. A good scope should be easily adjustable in both vertical and horizontal directions. A weighted or wide colposcope base prevents inadvertent tipping of the scope and damage to the head or to the optics. Most colposcopes are mounted on wheels, but platform/universal joint bases also are available. The choice of mounting system depends on examination room space requirements, need for mobility, and the colposcopist's preference. A colposcope usually has a powerful light source, with a rheostat to adjust the level of illumination. Spare light bulbs should be easily accessible since they may have to be changed during a procedure. Bulbs can be halogen, xenon, tungsten, or incandescent. Halogen bulbs produce a strong white light and are often preferred by colposcopists. Some colposcopes have bulbs mounted in the head of the scope, while others are mounted elsewhere and the light is delivered via a fiberoptic cable to the head of the colposcope. Scopes with fiberoptic cables can utilize hotter brighter bulbs, but the cables can be damaged if twisted or bent, producing less overall illumination. The colposcope should be equipped with a green or blue filter (red-free filter). These filters remove red light, thereby enhancing vascular detail by making the blood vessels appear dark. There are numerous options available for many of the scopes, and the prices are often subject to discounts. WHEC does not endorse or recommend either specific colposcopes or manufacturers. Scopes are warranted for variable lengths of time. Multimedia AccessoriesWhen the colposcope was first developed, the colposcopist would visualize the cervix and then make a drawing of normal and abnormal findings in the patient's chart. The system for making and labeling drawings has become more standardized since that time, but making a drawing of colposcopic findings in the medical record remains the standard of care for documenting the colposcopic examination. Indeed, some medical-legal experts have expressed an opinion that routine colpophotographs can increase legal risk because an "expert" can always be hired who can find something wrong in almost any photograph (5). However, with the advent of better optics and charged-coupled device (CCD) cameras, more options are now available to the colposcopist for documentation and education. Photographic and digital video-printers can produce permanent records of the exact pathology found. Recently, computers have been added to the system to allow fully computerized medical records, complete with digital photographs and the capacity for doing telemedicine. Multimedia accessories can be added to colposcopes through three major mechanisms. The simplest method of attaching a light-sensitive device to a colposcope is to replace an eyepiece ocular with a camera or a device that redirects the light path to a camera or other viewing apparatus. Unfortunately, this sometimes removes this light channel from use for stereoscopic viewing. Another method of adding multimedia accessories is to have an independent optic system supplying a separate optic port that can have a teaching tube, camera, or CCD video or photographic camera attached. Since the multimedia light channel and the viewing channels must have a completely separate set of lenses and objectives, this adds cost, and the accessory port often has only one magnification level regardless of the number of magnification levels of the viewing ports. The most popular method of adding accessory multimedia ports is via the use of a beam splitter. The beam splitter actually splits a light beam in half and sends the image to two separate ports, one to a viewing port and one to an accessory port. The advantage of this arrangement is that both ports present essentially the same image at the same time. This is especially useful in teaching with teaching tubes or video, since the teacher and learner see the same image at the same time. It also provides the patient with the added benefit of the teaching colposcopist's experienced assessment and input during the procedure. ColpophotographyColpophotographic systems are useful for documentation of treatment results or pathology that may have to be followed serially over time. They produce more detailed records of pathology than hand-drawings and can be useful with documenting and consulting on unusual findings. They also produce permanent images that can be useful in educating patients and colposcopy trainees. Colpophotographs can be retrospectively checked against pathology results to hone the colposcopist's ability to grade lesions. When using colpophotography, a permanent camera port is desirable so that fewer image opportunities are missed while finding or attaching the camera to the colposcope. Most colposcopes permit the use of a 35mm or Polaroid camera. Some systems make use of high intensity strobe flashes, which allow for higher shutter speeds that decrease the common problem of blurring on the image due to movement of the colposcope or the patient. Some manufacturers also have cameras available with data systems that record vital patient information onto the colpophotographs. Remote hand or foot shutter release switches are useful in decreasing blurring due to inadvertent motion during shutter activation. Digital colpophotography is being introduced. Some colposcopes have an eyepiece replaceable digital camera that can be used as a normal digital camera or may be put into the eyepiece port of a microscope or colposcope. Other colposcopes have an attachment that fits most beam-splitters and allows attachment of certain commercially available digital cameras. VideocolposcopyVideocolposcopy systems can be used for the same purposes as colpophotography, with the added advantage of real-time discussion of pathology with patients or trainees. Co-visualization can allow the patient to become aware of normally inaccessible anatomy. By allowing visualization and the opportunity to ask questions, patients may feel some control over the procedure, thereby decreasing anxiety. It also provides higher levels of patient satisfaction. In addition, the patient has the added benefit of a teaching colposcopist's experienced assessment and input during the procedure. Computerized ColposcopyWith the advent of modern CCD cameras attached to digitizing boards, it became possible to create high-resolution digital images of the cervix that could be displayed real-time, or (along with pertinent patient and examination data) stored, printed, or manipulated by a computer. The image captured can be reviewed and recaptured if suboptimal, unlike with colpophotography where the photograph is developed at a later date. Areas of interest can be enlarged, enhanced, or measured. Images also can be stored and retrieved for comparison at future visits or for consultation with expert colpscopists. As medicine moves toward more computerization of medical records, computerized colposcopy allows for easier integration into the electronic medical records. Computerized digital image processing may also facilitate a more quantitative method for following dysplastic lesions over time. Studies are being done on computer-assisted colposcopy, which may help improve training and the accuracy of colposcopic impression (7). Many computerized colposcopy systems were originally stand-alone systems made for colposcopy, but integrated systems have now been developed. InstrumentsVisualization of the cervix is one of the most critical technical components of the colposcopy procedure. Numerous vaginal specula are available for this purpose. A medium Grave's speculum is appropriate for most women. Pederson specula have narrow blades for use in virgins (rare in colposcopy) and women with a narrow vaginal diameter. A large metal Grave's speculum may be required for obese women, pregnant women, and women with vaginal wall laxity. Women with an extremely long vagina may require the use of a long Grave's or Pederson speculum. The light source from the colposcope may be used for vaginal speculum insertion. Internally illuminated plastic speculums may also be used but tend to have thinner blades than standard Grave's speculums. If the patient has extremely lax vaginal walls, lateral vaginal side-wall retractors can be helpful. The use of these instruments requires a degree of skill, for if proper perpendicular alignment with the vaginal speculum is not maintained, severe vaginal pinching occurs. Alternatively, a condom, a penrose drain, a latex ultrasound vaginal probe sheath with the end removed, or the cut middle finger or thumb of a latex glove with the end removed can be placed over the speculum blades to gently hold the side-walls back and allow better visualization of the cervix and vaginal fornix. The purpose of colposcopic biopsy forceps is to take a small but adequate tissue sample of lower genital tract tissue. Many types of biopsy forceps have been developed. The four most common types of forceps used in the United States are the Tischler, Baby Tischler, Eppendorfer, and Kevorkian biopsy forceps. WHEC does not endorse or recommend specific brands, specific forceps or other sampling instruments. To obtain a satisfactory colposcopy, visualization the entire squamo-columnar junction (SCJ) is necessary. When the SCJ or part of a lesion recedes into the endocervical canal, the colposcopist may need to apply pressure near the os with a cotton-tipped applicator in order to open the canal. If this is not adequate for visualization, an endocervical speculum may be necessary. Kogan endocervical speculum: Blades typically come in 2mm, 4mm or 6mm sizes. The blades may be inserted into the cervical os and gently opened to allow better visualization. The blades of the endocervical speculum are inserted into the canal to gently retract tissue for proper visualization. This procedure is usually not painful unless the os is stretched. Several of these instruments should be made available, since a size should be selected for each patient that is large enough to allow visualization but not so large that it stretches the os. Endocervical speculums come in several sizes, from 2mm for stenotic os to 6mm for large parous os. Some colposcopists remove the thumbscrews or ratchet lock on the endocervical speculums to allow more dynamic and precise control of the instrument. Visualizing the squamocolumnar junction was formerly used to triage women with cervical intraepithelial neoplasia (CIN) to ablative (laser, cryotherapy) or excisional (Large Loop Excision of Transformation Zone [LLETZ], cold cone) treatment (8). While unsatisfactory visualization of the SCJ still mandates excisional therapy, women with a deep but visible SCJ also may need excisional therapy when available ablation treatments cannot reach far into the endocervical canal. Chemical AgentsSeveral solutions are used during the colposcopic exam. Normal saline is used as a moistening and cleansing solution during colposcopy. It does not alter the cervical epithelium. It is usually obtained in standard stock bottles from suppliers or from drug stores. Acetic acid (3%-5%) is used as a contrast solution to enhance the detection of cervical neoplasia during the colposcopic examination. It can be obtained from a supermarket as white vinegar or from a medical supply source. It may be slightly diluted to a 3% solution in an attempt to decrease the stinging sensation to the patient, but this also decreases its time of action on the cervix. Most colposcopists use undiluted 5% solutions. Aqueous Lugol's solution is an iodine-based contrast solution that is mainly used when examining the vagina, but it may also be used in cervical colposcopy. Lugol's solution is less irritating and just as effective when diluted to half-strength by adding an equivalent amount of tap water or saline. Patients always should be asked about a potential iodine allergy before application of Lugol's solution. Monsel's solution (ferric subsulfate) is the most common hemostatic agent used after lower genital tract biopsy or excision. It performs best when it has a thick, toothpaste consistency. It can be bought this way or produced by allowing the stock solution to sit exposed to the air in a small open container. This allows evaporation and thickening of the agent, a process that can be enhanced by placing the open container in a warm place, such as on top of a refrigerator. The resulting paste texture can be maintained by keeping the paste in a closed container and by adding small amounts of Monsel's solution whenever the paste becomes excessively thick. Application of silver nitrate sticks and gelatin foam/powder are less commonly used methods of hemostasis. 2011 Colposcopic Terminology of the CervixThe colposcopic examination should be assessed for three variables:
General AssessmentThe popular terms "satisfactory colposcopy" and "unsatisfactory colposcopy" have been replaced. "Adequate or inadequate for the reason": this should be the opening statement of every colposcopic examination. The examination may be inadequate because the cervix is obscured by inflammation, bleeding, or scarring. Squamo-columnar junction visibility: the squamo-columnar junction may be completely visible when 360° of the squamo-columnar junction is seen and partially visible when most of the squamo-columnar junction is visible but a section of it is inside the endocervical canal or when a lesion covers the squamo-columnar junction with its inner border in the endocervical canal. The squamo-columnar junction may not be visible when all or most of the squamo-columnar junction cannot be seen because it is in the endocervical canal. It can be described as "completely visible", "partially visible", or "not visible". The reason that the visibility and site of the squamo-columnar junction are so important is that it dictates the ability to do a satisfactory examination and, when treatment is indicated, the extent and type of excision. The terms "adequacy" and "squamo-columnar junction visibility" are not mutually exclusive. For example, the squamo-columnar junction may be "partially visible" because a portion of its inner margin is located high in the endocervical canal, whereas the test is still "adequate" because the cervix itself is not obscured by blood or inflammation. The third parameter involves assigning a transformation zone type (9). It overlaps to some degree, but not completely, with the visibility of the squamo-columnar junction. The transformation zone and the squamo-columnar junction are not the same thing: the squamo-columnar junction is the "inner" margin of the transformation zone. Both types 1 and 2 transformation zone are "completely visible", but the differentiation between two may be important, mainly for planning treatment. Updated Colposcopic Terminology of the Cervix
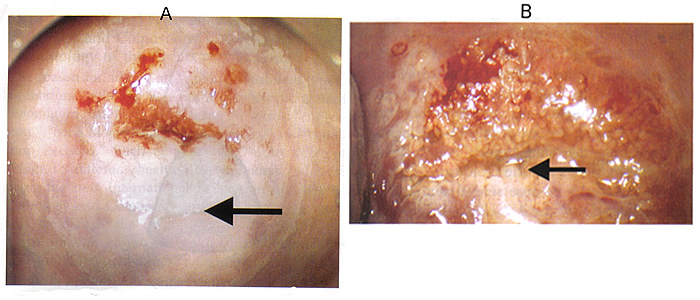 Fig. 1 Abnormal colposcopic findings; location of the lesion inside or outside the transformation zone. A: Inner border sign. The arrow points to the sharp demarcation between thin and dense acetowhite areas that exists within the same lesion. B: Ridge sign. The arrow points to the opaque protuberance that is present at the area of a white epithelium within the transformation zone. Abnormal Colposcopic FindingsLocation of the lesion is relative to the original squamo-columnar junction. "Inside" location means medial to the original squamo-columnar junction (towards the cervical os) and vice versa. The border of a lesion is a sharp border that is a straight edge of an acetowhite cervical lesion. Other edge definitions are feathered or geographical margin, usually associated with a low-grade lesion, and rolled peeling edges that may be associated with a high-grade lesion (1). The inner border sign is a sharp demarcation between thin and dense acetowhite areas within the same lesion (as shown above). The ridge sign (13) is an opaque protuberance at the area of a white epithelium within the transformation zone (as shown above). In the "abnormal colposcopic finding", the localization of the lesion to either inside or outside the transformation zone has been added in the terminology. A lesion within the transformation zone, as opposed to one outside, has been shown to be an independent predictor of a high-grade lesion or carcinoma (10). The size of the cervical lesion has been found to have a predictive value for a high histologic grade (11). Therefore, several determinants of size as well as of location of cervical lesions are included in this latest terminology: the number of cervical quadrants the lesions covers, size of the lesion as a percentage of the cervix, and location of the lesion by clock position(s). All three parameters are incorporated into the terminology because the parameters of size and location do not overlap; for example, a lesion can occupy three quadrants but be composed of a thin layer of abnormal epithelium that occupies only 5% of cervix. It may extend for the 2 o'clock to the 8 o'clock positions. Introduction of the two new signs, "inner border sign" and "ridge sign" to the grade 2 (major lesions) section is the result of their significant validity as markers of high-grade cervical intraepithelial neoplasia (12),(13). Sharp border has also been associated with a more severe lesion. The term leukoplakia or keratosis is considered a major lesion in the terminologies because leukoplakia or keratosis is shown to have a 25% independent predictive value of containing high-grade or invasive neoplasia (14). Non-specific category may represent either a benign or a severe intraepithelial lesion. Moving the test of Lugol's staining (Schiller's test) from the "minor grade" category to the "non-specific" category of the "abnormal colposcopic findings" section is because several studies such as those associated with the ASCUS-LSIL Triage Study showed poor reliability of Lugol's staining (15)(16). A cervical polyp is a common finding and is in the "miscellaneous findings", including its origin as being ectocervical or endocervical. Miscellaneous findings: Post-treatment effect may or may not be an adverse feature; for example, stenosis, deformation or distortion, scarring, thickening or increased fragility of the mucosa, cervical endometriosis. Updated Colposcopic Terminology of the Vagina
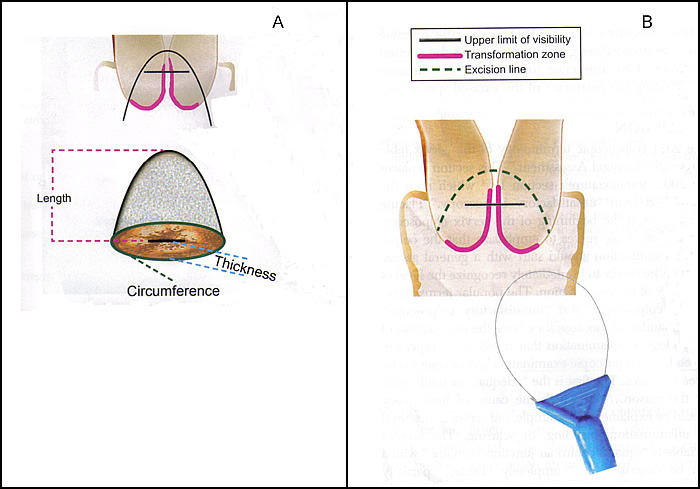
Updated Colposcopic Terminology of the Cervix - AddendumThe reason for adding a "excision treatment types" addendum is to avoid using terms: "conization," "cone biopsy," "big loop excision", and "small loop excision." Each of these may mean different things to different health care providers, whereas using the new IFCPC excision treatment types will standardize the descriptions of the transformation zone. The excision of each of the transformation zone types is associated with a different technique as well as altered risk of incomplete excision and subsequent morbidity. The rationale for inclusion of the excised specimen dimensions in the 2011 IFCPC terminology is similar. Several studies have shown that the size of the excised specimen of the cervix has implications on future pregnancy outcome. Therefore, there is a need to standardize the description of the excised specimen dimensions (17). There is a lack of consensus in the published literature concerning the terms "length," "depth," and "height" of the specimen. In some publications "length" means the distance from the ectocervical margin to the endocervical margin. In other articles this parameter is termed "depth" or even "height." To clarify this, the proposed terminology advises abandoning the term "depth" and "height" and instead proposes the terms "length" and "thickness" (17).When multiple excision specimens are obtained, as is the case with an endocervical top-hat specimen, each specimen will be measured separately. Fig. 2. Colposcopic terminology of the cervix - addendum: Excision treatment types. A: Line drawing of a large loop excision of the transformation zone specimen after removal, with dimensions used to designate thickness, length, and circumference. B: Type 3 excision. Resection of a type 3 transformation zone. It includes a longer and larger amount of tissue than type 1 or type 2 excisions and a significant amount of endocervical epithelium. The excision types corresponding to the transformation zone-type classification describes three types, which are classified according to the site, size, and visibility of transformation zone. The excision itself may be carried out by any of the accepted methods: large loop excision of the transformation zone (LLETZ), which is identical to loop electrosurgical excision procedure, by needle excision of the transformation zone, by straight wire excision of the transformation zone, or by cold knife conization. Type 1 excision: It resects a completely ectocervical or type 1 transformation zone. Type 2 excision: It resects a type 2 transformation zone. It will resect a small amount of endocervical epithelium that is visible with a colposcope. Type 3 excision: It resects a type 3 transformation zone. It will resect a longer and larger amount of tissue than type 1 or type 2 excisions and will include a significant amount of endocervical epithelium. It may also be used to treat glandular disease or microinvasive disease or women who have had previous treatment. The International Federation of Cervical Pathology and Colposcopy recommends that the 2011 terminology replace all others and be implemented for diagnosis, treatment, and research. The popular terms "satisfactory colposcopy" and "unsatisfactory colposcopy" have been replaced. The colposcopic examination should be assessed for three variables: 1) adequate or inadequate, with the reason given; 2) squamo-columnar junction visibility; 3) transformation zone type. Other additions were the localization of the lesion to either inside or outside the transformation zone and determinants of size as well as location of cervical lesions. Two new signs are included in the terminology - the "inner border sign" and "ridge sign". The following definitions have been added: congenital transformation zone, polyp (ectocervical or endocervical), stenosis, congenital anomaly, and post-treatment consequence. In addition, the terminology includes standardization of cervical excision treatment types and cervical excision specimen dimensions. International Federation of Cervical Pathology and Colposcopy (IFCPC) 2011 Colposcopic Terminology The series on Cervical Cancer Prevention was funded by WHEC Initiatives for the Global Health. This program is undertaken with the partners of Women's Health and Education Center (WHEC) to eliminate/reduce cervical cancer worldwide. Contact us if you wish to contribute and/or join the efforts. |